Frozen shoulder, or adhesive capsulitis, is a condition that causes stiffness, pain, and restricted range of motion in the shoulder joint. As a sports massage therapist, understanding how to identify and treat this condition is vital for helping clients regain mobility and reduce discomfort.
This blog will explore the causes, symptoms, and stages of frozen shoulder, followed by practical massage therapy techniques and tips for effective treatment.
UNDERSTANDING FROZEN SHOULDER
What Causes Frozen Shoulder?
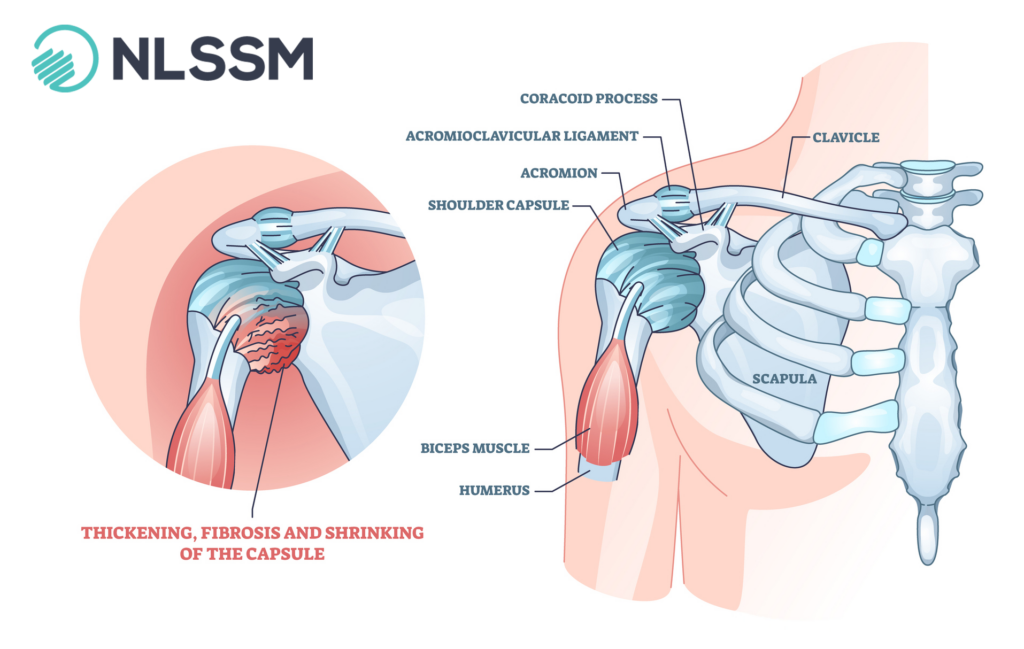
Frozen shoulder occurs when the connective tissue surrounding the shoulder joint thickens and tightens, leading to reduced mobility. Common causes can be seen split into two groups and typically include:
Primary / Idiopathic:
Metabolic conditions (Type II Diabetes) account for 10%-36% of cases (2), as other conditions such as Parkinson’s, previous stroke, Thyroid
Secondary:
Traumatic incidence (is it impingement?)
Non-traumatic – osteoarthritis, rotator cuff tendinopathy
It is rare to develop Frozen Shoulder under the age of 40, the peak age is 56 (1). It typically affects more women than men.
Red Flags: If over 60 and presenting with capsular restriction, think Osteoarthritis first.
SYMPTOMS AND STAGES
The condition typically progresses through three clinical stages.
- Freezing Stage: Acute
- Pain increases gradually, and shoulder movement becomes limited.
- Duration: 6 weeks to 9 months.
- Freezing Stage: Sub Acute
- Pain may subside, but stiffness remains, significantly limiting range of motion.
- Duration: 4 to 12 months.
- Thawing Stage: Chronic
- Gradual return of mobility as the connective tissue loosens.
- Duration: 6 months to 2 years.
Recent research shows that only 59% of patients regain full function within 4 years (Wang et al., 2016)
INITIAL ASSESSMENT
The diagnosis of Frozen Shoulder is a clinical one (Physical) rather than diagnostic i.e. x-rays. A diagnosis should be undertaken by the patient’s doctor or physiotherapist. Their assessment will involve the following:
- Range of Motion Tests: looking at the capsular pattern in the shoulder lateral rotation, abduction and medial rotation (LAM). Taken through the passive range and then actively.
- Palpation: Assess muscle tension, adhesions, or trigger points around the shoulder girdle.
- Client History: Understand any underlying causes, such as prior injuries or medical conditions.

SO, HOW DO YOU TREAT FROZEN SHOULDER?
The simple answer is that you don’t.
However, there is a lot we can do as soft tissue therapists to help support our client’s journey through their experience.
- Go global: Help maintain mobility of the unaffected shoulder and surrounding structures of the affected shoulder.
- Pain regulation: Downregulate the nervous system. Help to assist in reducing the sympathetic nervous system firing.
- Client engagement: Help to reduce frustration and improve compliance by engaging your client in the process. Incorporating education around their activities can be really important i.e. sleeping position, can they choose some exercise that is pain free.
- Language: We need to be mindful of the discussion around the client’s pain and their perception of pain. Positive reinforcement is encouraged.
MASSAGE TECHNIQUES
Your techniques and their application will depend on the presenting stage of the client’s Frozen Shoulder.
Acute
- Techniques should be slow and considered: General Massage techniques such as effleurage, petrissage, compression
- Reduce hypertonicity and trigger points in and around the pectoralis major & minor, subclavius, deltoid, and bicep. Help assist in maintaining local circulation
- Look at Diaphragmatic breathing – breathing patterns could be impacted due to pain – Muscle Energy Technique is an effective non-invasive approach.
- Help maintain mobility of the unaffected shoulder, look at compensatory patterns.
Sub-Acute/Chronic
- The approach can be broader with still using the same techniques as the acute stage – effleurage, petrissage, compression.
- Remedial techniques such as Trigger Point Therapy (TrP), Transverse Soft Tissue Release (TSTR), Myofascial Release (MFR)
- ‘Stretching’ should be slow & well-supported – think of using something like Muscle Energy Technique (MET). Treat the capsule-like gum. Pull too quickly, it snaps, pulls, and moves slowly, lengthens and gives
Remember: Positioning of your client is key! Support of the affected shoulder must always be undertaken so that they are pain-free on the table. All techniques should be applied in a pain free manner to the client.

OTHER THERAPIES
- Heat Therapy: Use heat packs before massage to relax muscles and improve circulation.
- Ultrasounds Guided Injection: Performed by a doctor or qualified physiotherapist.
- Active Release Techniques: Combine active movements with targeted pressure to address specific muscle groups.
OTHER EFFECTIVE TIPS
- Communication:Regularly check in with your client to gauge their pain levels and comfort during the session.
- Custom Treatment Plans: Adjust techniques and pressure based on the client’s current stage of frozen shoulder.
- Home Care Advice: Recommend gentle exercises, such as pendulum swings or wall walks, to maintain mobility between sessions. Advise on using heat or cold therapy as needed.
- Collaborative Care: Work alongside physiotherapists or medical professionals if the client requires multidisciplinary support.
CONCLUSION + FURTHER LEARNING
Frozen shoulder can be a challenging condition, but with the right approach, sports massage therapists can play a pivotal role in their clients’ recovery journey.
By combining targeted techniques with a personalised treatment plan, you can help clients regain mobility, reduce pain, and return to their active lifestyles.
Further Learning
For further learning in this area, we have a couple of options for you.
- Join our Treating the Shoulder CPD Practical Workshop + online course where we look at conditions like frozen shoulder and more. Click here for more information.
- We also have a webinar available for rent in our Video Library: Frozen Shoulder: Role of Manual Therapy – Friend or Foe? Check out a short preview of the webinar below and find out more by clicking here.
REFERENCES
- Zuckerman, J. D., & Cuomo, F. (1993). “Frozen shoulder: Diagnosis and management.” The Journal of the American Academy of Orthopaedic Surgeons, 1(4), 240-249.
- Kelley, M. J., & McClure, P. W. (2009). “Frozen shoulder: Evidence and a proposed model guiding rehabilitation.” The Journal of Orthopaedic & Sports Physical Therapy, 39(2), 135-148.
- Cyriax, J. (1982). Textbook of Orthopaedic Medicine: Volume 1. London: Baillière Tindall.
- Neviaser, R. J. (1987). “Adhesive capsulitis of the shoulder: A study of the pathological findings in periarthritis of the shoulder.” The Journal of Bone and Joint Surgery, 27(2), 211-222.
- Bunker, T. D. (1997). “Frozen shoulder: Unravelling the enigma.” Annals of the Royal College of Surgeons of England, 79(3), 210-213.
